From Data to Decisions: Leveraging CDSS for Safer Patient Care
Medical decisions have never been more difficult. Clinicians must manage thousands of pharmacological combinations, shifting recommendations, and massive amounts of real-time data. Preventable medical mistakes are the third-leading cause of mortality in the U.S, accounting for about 250,000 deaths annually. Clinical decision support systems offer alleviation.
By incorporating evidence-based logic, AI, and patient-specific data into daily workflows, these tools provide the right insight at the right time, significantly improving patient outcomes.
In this blog, you’ll learn what CDSS technology is, how it works inside EHRs, and what actions healthcare executives may take to properly use it.
What is a Clinical Decision Support System?
A CDSS is a software that analyzes patient-specific data from labs, vitals, and history, which provides context-aware recommendations inside an EHR or other point-of-care workflow. Classic rule-based alerts are increasingly coexisting with AI engines that identify differential diagnoses, propose order sets, and detect small pattern changes.
Whatever the methodology, the purpose is the same: to provide evidence-based treatment, eliminate medical mistakes, and enhance patient outcomes.
Core Building Blocks
- Clinical guidelines, pharmacological databases, and prediction models all form part of the knowledge base.
- Inference engines are logical rules or machine-learning algorithms that compare patient data to a knowledge store.
- The communication layer is the on-screen alert, dashboard, or automated order that reaches physicians without disturbing care.
How CDSS Enhances Patient Outcomes
CDS technologies that have been properly deployed routinely transfer information into significant clinical benefits.
- According to a recent comprehensive analysis, computerized CDSSs reduce medication mistakes and adverse drug events with moderate confidence.
- Hospitals that included early-warning sepsis signals in their EHRs found significant decreases in mortality within a year.
- Particularly in high-volume crises, AI-guided differential diagnostic help minimizes missing or delayed diagnoses.
- Evidence-based bundles such as heart-failure core measures or VTE prophylaxis are encouraged to be followed by point-of-care care pathways.
Fewer errors, faster interventions, and stricter adherence to best practices all contribute to higher patient survival rates, shorter lengths of stay, and lower readmission rates.
Essential Capabilities in Modern CDS Tools
1. Real-time Clinical Notifications – Check for allergies or medication interactions. Early warning scores for sepsis, acute kidney injury, and stroke.
2. Machine Learning and Predictive AI – Risk categorization for readmission or worsening. Using natural language processing to mine free-text notes
3. Evidence-based Order Sets and Care Pathways – One-click orders that pre-populate labs, imaging, and medications according to guidelines
4. EHR Connection is Seamless – FHIR and SMART-on-FHIR APIs to maintain data flow and prevent double-documentation
5. User-Defined Alerting – Adjustable thresholds, role-specific filters, and “silent mode” for non-urgent insights can help fight alert fatigue.
Integration – Where CDSS Meets EHR
Integration is the distinction between a life-saving nudge and an ignored pop-up. Best-practice deployments:
1. Utilize Open Standards – Modern suppliers include FHIR-based endpoints and CDS Hooks, allowing the tool to read vitals, labs, and orders in milliseconds.
2. Embed Natively – Recommendations should show within the clinician’s existing EHR workspace, with no additional logins required.
3. Write Back Data – Accepted alerts should automatically document the intervention, thereby completing the loop on quality reporting.
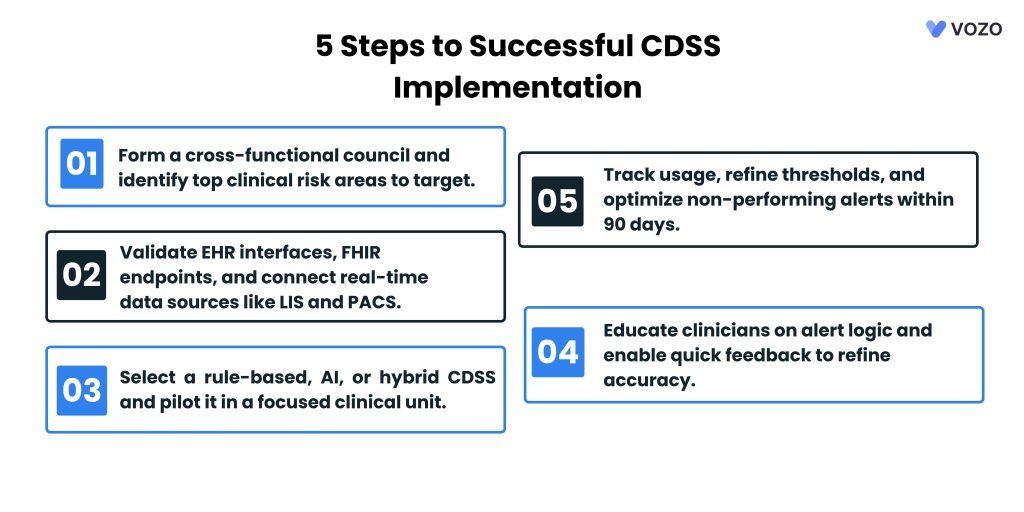
Implementation Roadmap
1. Stakeholder Alignment
- Organize CMOs, pharmacists, frontline nurses, and informatics professionals into a single governing council.
- Identify 3-5 high-risk areas, such as sepsis delays and anticoagulant dose adjustments.
2. Data & Integration Readiness
- Examine EHR interfaces and validate FHIR endpoints.
- Map the downstream systems, such as LIS and PACS, that provide real-time data.
3. Choose and Configure the Engine
- Rule-based, AI-guided, or hybrid? Weigh openness against flexibility.
- Start with a pilot unit to fine-tune the thresholds.
4. Clinician Training & Change Management
- Walk attending physicians through alert logic and demonstrate evidence sources.
- Provide a “one-tap feedback” button so that consumers may rapidly report false positives.
5. Monitor, Measure, and Iterate
- Track alert acceptance rate, override causes, and result shifts monthly.
- Retire or modify restrictions that do not enhance care within 90 days.
Measuring Success: Metrics That Matter
| Metric | Why It Counts |
| Alert Acceptance | High acceptance signals relevance; low rates highlight noise |
| Time to Critical Therapy | Minutes from alert → first dose, such as an antibiotic, correlates with survival |
| Adverse Event Rate | Watch falls, ADEs, or code blues per 1,000 encounters |
| Clinician Satisfaction | Short “pulse” surveys reveal fatigue or trust gaps |
| ROI | Compare avoided harm costs versus licensing and upkeep fees |
Market Outlook and Strategic Rationale
Healthcare purchasers are voting with their wallets. The worldwide CDSS market is expected to reach $16.7 billion by 2030, up from $10.8 billion in 2024 a 7.6% CAGR powered by value-based care incentives and AI advances.
Early adopters achieve a competitive advantage by:
- Capturing quality bonus monies linked to evidence-based criteria.
- Reducing malpractice exposure with well-documented, guideline-aligned judgments
- Freeing clinician bandwidth, a critical advantage in tight labor markets.
Common Pitfalls and Quick Fixes
1. Alert Fatigue – Pop-ups lose their effect when every tiny issue triggers an alarm. Tier alerts ensure that only high-risk events are disrupted.
2. Data Silos and Integration Gaps – Incomplete feeds stifle suggestions. Connect systems to FHIR APIs to ensure real-time data flow.
3. One-size-fits-all thresholds – Generic rules do not apply consistently across specialties. Adjust cut-offs by unit and patient group.
4. Shadow IT Workarounds – Old CDS system directs physicians to unapproved applications. Co-design features and iterate quickly to keep people engaged.
5. Regulatory and Liability Blind Spots – Models that are opaque and have missing logs invite investigation. Maintain audit logs and validate algorithms once a year.
Related: 10 Ways AI-Driven Clinical Decision Support Systems Reducing Medical Errors in Top US Hospitals
Vozo Cloud EHR with Clinical Decision Support System
From digitizing patient records to minimizing medical errors, Vozo EHR empowers providers to make faster, smarter clinical decisions that elevate care quality.
If you’re seeking an EHR system that goes beyond data entry to actively support clinical judgment, Vozo EHR is your trusted partner.
With Vozo Cloud EHR, practices of all sizes benefit from a cost-effective subscription model and scalable infrastructure.
Our specialty-specific features—including lab integration, patient portals, scheduling tools, and cloud hosting—are designed to reduce administrative burden and enhance clinical efficiency.
Vozo Customized EHR with built-in CDS helps your practice:
- Improve decision-making with evidence-based prompts and alerts
- Streamline documentation and reduce errors
- Access consolidated patient data anytime, anywhere
- Boost operational efficiency and cut unnecessary costs
And with our expert support team available 24/7, help is always just a click away.
Choose Vozo EHR to simplify decisions, reduce clinical risk, and focus on what matters most—patient care.
About the author

With more than 4 years of experience in the dynamic healthcare technology landscape, Sid specializes in crafting compelling content on topics including EHR/EMR, patient portals, healthcare automation, remote patient monitoring, and health information exchange. His expertise lies in translating cutting-edge innovations and intricate topics into engaging narratives that resonate with diverse audiences.