How AI Scribes Can Cut Documentation Time by 50%
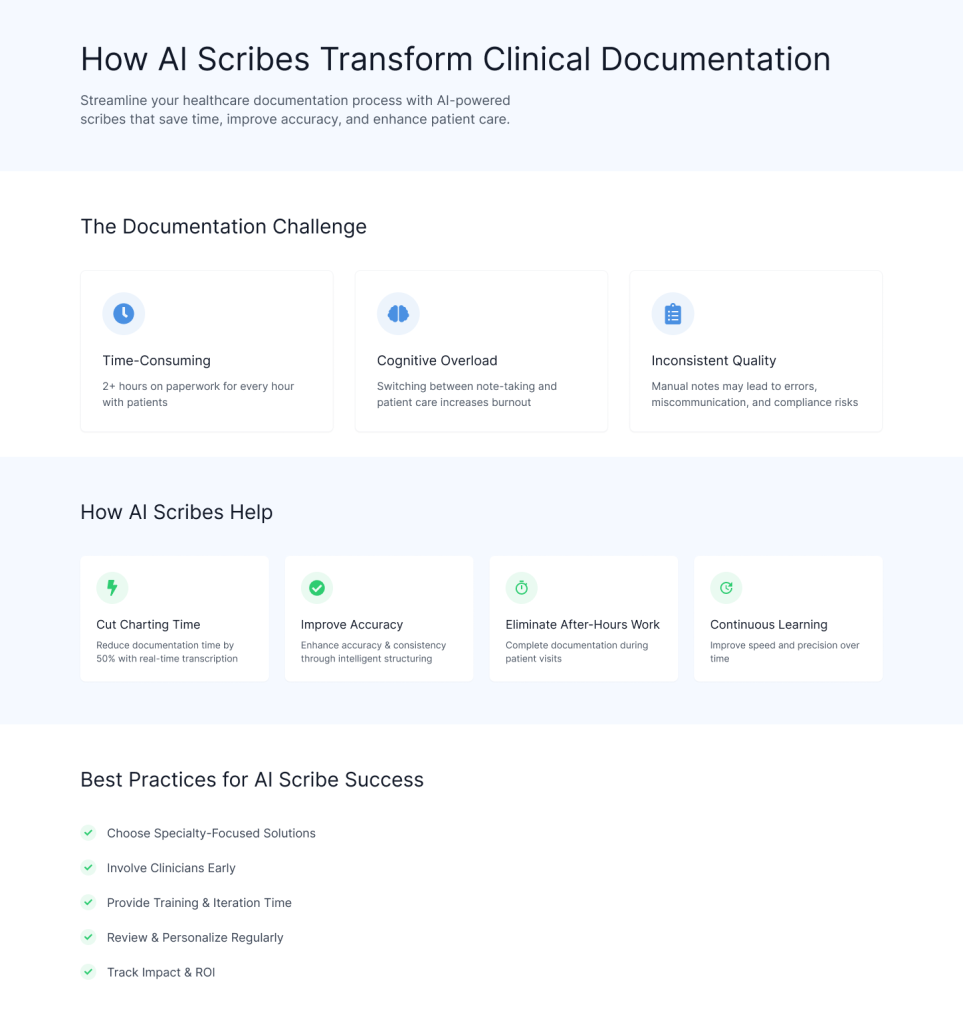
Clinical documentation is an important process, yet time-consuming in modern healthcare. Physicians and other caregivers frequently spend more than two hours on paperwork for every hour spent with patients, resulting in burnout, less face-to-face time, and higher operating costs.
AI-powered digital assistants help in medical documentation by lowering charting time by up to 50%, decreasing burnout, and boosting clinician-patient relationships.
In this blog, you’ll learn the challenges and best practices of how AI scribes can reduce documentation time by integrating into the clinical process, freeing clinicians to focus on patient care.
The Rise of AI Scribes in Healthcare
- AI scribes employ advanced technology such as speech-to-text engines, machine learning, and natural language processing to autonomously document clinical interactions.
- They “listen” to the clinician-patient dialog, transcribe it with high accuracy, and intelligently structure the material into EHR-compatible notes.
- Some complex systems also offer diagnosis codes and treatment recommendations based on the discussion, saving time and increasing uniformity.
Challenges in Medical Documentation
1. Time Drain
According to surveys, clinicians spend over half of their working hours documenting EHR. Administrative tasks limit direct patient engagement, reducing rapport and satisfaction.
2. Cognitive Load
Switching between patient talk and note-taking disrupts concentration and promotes mental weariness. High paperwork loads are associated with burnout and turnover.
3. Variability of Quality
Handwritten or manually inputted notes may be inconsistent, fragmentary, or lacking in organization. Ineffective documentation raises the possibility of misinterpretations, coding mistakes, and compliance issues.
4. Workflow Disruption
Traditional scribes need training, coordination, and additional expenses. Hiring human scribes is not scalable across all specialties or practice sizes.
Related: How AI Cuts Down Medical Documentation Time by 2 Hours Every Day for Providers
How AI Scribes Reduced Documentation Time by 50%
1. Parallel Processing of Documentation
- While the practitioner attends to the patient, the AI scribe records and creates the notes behind the scenes. This parallelization effectively reduces the time required to write up after a visit.
- By arranging information into established templates, AI scribes reduce the laborious sorting and formatting that physicians often do.
2. Reduction in Manual Review
- Modern NLP algorithms achieve up to 95% transcribing accuracy, physicians simply require quick overviews and minor revisions rather than creating notes from scratch.
- AI emphasizes critical discoveries, anomalous numbers, and decision points, allowing providers to validate instead of recreating material.
3. Elimination of After-Hours Work
- Notes are created at the point of care, which eliminates the need for late-day or weekend documentation sessions.
- Sign-off is faster since templates are pre-populated and ready, making it a click-based process rather than a typing marathon.
4. Continuous Learning and Improvement
- AI scribes learn from physician modifications to improve terminology, template usage, and specialty-specific language. This feedback loop gradually reduces review time.
- Deep integration requires fewer clicks to import and export data, reducing navigation and selection time inside complicated EHR interfaces.
Addressing Common Concerns
1. Accuracy and Liability – Clinicians check AI transcripts before they are signed. The responsibility lies with the supplier, not the AI.
Many systems provide “confidence scores” for transcribed parts, indicating places that require further evaluation.
2. Patient Privacy – Enterprise-grade scribes follow HIPAA and GDPR guidelines, using end-to-end encryption, secure cloud storage, and role-based access restrictions.
3. Workflow Disruption – Begin with a small cohort to fine-tune microphone positioning, template preferences, and user training.
Systems can be tailored to certain lexicons, such as cardiology vs. dermatology, to ensure maximum relevance from the start.
4. Cost and ROI – While there is an initial subscription or license charge, ROI is achieved through improved billing capture accuracy, increased throughput, and lower clinician burnout-related turnover costs.
AI Scribe for Clinical Documentation
Best Practices for Implementing AI Scribe
1. Select a Specialty-Focused Scribe Solution
- Choose AI scribe vendors who provide specialty-specific templates and language models customized for your clinical area.
- Ensure that the system can be tailored to your workflow, documentation style, and compliance requirements for improved accuracy and uptake.
2. Engage Clinicians Early
- Include clinicians, nurses, and key staff in the selection, design, and pilot testing phases to foster ownership and trust.
- Use early input to fine-tune templates and workflows that are consistent with real-world clinical practice.
3. Invest in Training and Time for Iteration
- Conduct extensive training sessions and establish realistic goals for progressive growth.
- Allow for continual learning and adjustment as the AI and clinicians acclimate to the new workflow.
4. Regularly Review, Update, and Personalize
- Regularly examine edit logs and user comments to detect patterns and make targeted changes.
- Update templates and terminology to suit changing clinical language and specialization demands to ensure long-term correctness.
5. Track Metrics and ROI
- Measure impact by tracking critical parameters such as documentation time, clinician satisfaction, and coding accuracy.
- Use data insights to optimize consumption, highlight value, and promote continuous improvement throughout the business.
Related: How HealthScribe AI Transforms Medical Charting with Real-Time Provider-Patient Conversation
Vozo EHR Integrated with Amazon Health Scribe
While many mistakes occur in EHR note-taking, you can easily rectify them by relying on the best electronic health records system. That’s why we built Vozo Cloud EHR, now seamlessly integrated with Amazon Health Scribe.
Our all-inclusive electronic health records system will make it easier for you to take notes during patient encounters with enhanced accuracy and efficiency. Moreover, Vozo EHR can be your first option if you’re looking for the best EHR system for your medical business.
Our all-inclusive EHR system simplifies and handles all the duties, allowing you to concentrate more on patient care.
- All practice levels benefit from an affordable cloud subscription to Vozo Cloud EHR.
- Our feature-rich EHR facilitates error correction and expedites the process.
- The needs and requirements of specialized practices are met by the Vozo specialized EHR.
- If you ever have any questions, our knowledgeable technical staff is here to help.
- As your healthcare facility expands, our EHR System keeps expanding to enhance the user experience.
The Vozo Customized EHR solution, integrated with Amazon Health Scribe, benefits your healthcare practice by streamlining the administrative process, improving workflow efficiency, reducing the risk of errors, and managing all patient records in one place, offering greater efficiency and cost savings across the board.
Our specialty-specific tools, like scheduling, patient portals, lab integration, cloud hosting, and more, meet the specific needs and requirements of your healthcare practice.
“Embrace Vozo EHR, enhanced with Amazon Health Scribe, to Reduce Your Burdens and Enhance Patient Care.”
About the author

With more than 4 years of experience in the dynamic healthcare technology landscape, Sid specializes in crafting compelling content on topics including EHR/EMR, patient portals, healthcare automation, remote patient monitoring, and health information exchange. His expertise lies in translating cutting-edge innovations and intricate topics into engaging narratives that resonate with diverse audiences.













